| New Directions in Childbirth - Empowering Birthers |
 |
| Written by Jamie McDonald |
| 04 June 2023 |
|
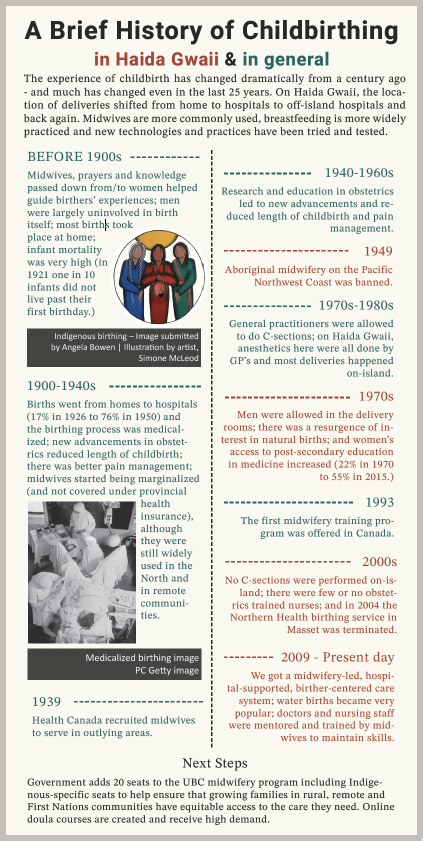
When I started interviewing birthers, doulas, midwives and doctors for this piece about the history of childbirth on Haida Gwaii, I found myself encouraged by the direction that seems to be taking hold here: a direction where forgotten and/or banned knowledge-holders are being reintegrated and valued, where choices are being offered and explained and where top-down power and control is being reversed. In past articles published in this magazine, we introduced readers to the various roles and local folks involved in the birthing process on these Islands. Now, we can see how they have been coordinated with the Western medical system to provide birthers with a supported, integrated, home-grown experience. To learn more about this development, I sat down with some islanders involved in childbirthing.
“I had my first birth in a hospital setting (off island), and as with all first experiences, I didn’t know what to expect. The pregnancy was past its term and the hospital staff wanted to induce labour. I had quite a traumatizing experience and didn’t feel like my birth plan was respected at all. The hospital room was flooded with so many (too many) people, but I couldn’t connect with anyone, they pushed on my stomach and pulled the baby out, the scissors were ready even when I had expressed wanting delayed cord clamping… hospitals have a place in birthing, but my experience led me to think that hospitals had an outdated way of going about it. My two subsequent birthing experiences happened on Haida Gwaii, with midwives and doulas, and were very healing. The midwives had lots of strategies to get labour going, they had the capacity to unhook a baby’s shoulders manually, they were able to be my advocates and made sure my birth plan was respected. With their support and knowledge sharing, they created a calming environment and allowed me to let go of a lot of fear I had.”
“It was such a gift to have had the opportunity to labour on-island with a midwife that was so comfortable letting things ride and not being so worried about protocol, and who made me comfortable to trust in her experience and my intuition. Midwives here are so amazingly confident, strong and empowering. This was one of the reasons we moved back to Haida Gwaii to give birth. There are still lots of jurisdictions where midwives don’t exist. In Prince George (where I used to live), even in the care of a midwife, I don’t know if I would’ve been supported in some of the decisions I made. Midwives here are used to things going a little differently. All of that allowed me not to have so many hard feelings about ultimately having to birth off island. Them holding space for me to give it a try for so long on island, in my home, was amazing.”
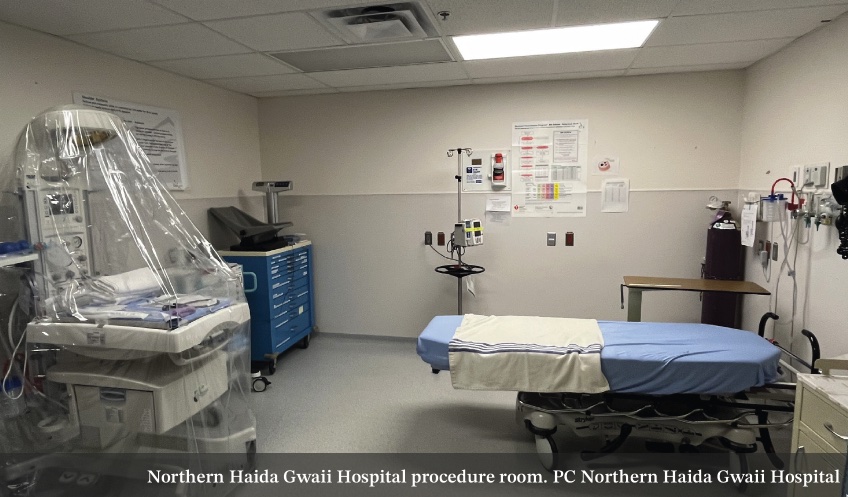
“Since there are no specialists on island, no surgical capabilities and no intensive care options for pregnant people or newborns and no anesthesia service, in general, approximately half of pregnant people from Haida Gwaii will plan to give birth on-island. All clients are counseled about the risk and benefit of on-island and off-island delivery, as well as in-hospital or out-of-hospital delivery. “Pregnancy and childbirth are intimate experiences with much unpredictability; set on a systemic stage of racial and gender inequities, including colonial trauma. Trusting connections between clients and providers that prioritize individual autonomy are paramount for healing. A decolonized approach to childbearing puts pregnant people at the center of the experience and amplifies Indigenous voices; pregnant people are the decision- makers and the systems adapt to their autonomous choices. People view midwives, doulas, home births, as part of the movement to decolonize childbirth. In my report called Haida Gwaii Maternity Program, A Rural/ Remote Maternity Service, Haida Gwaii, British Columbia, March 2021, I highlighted the need for prioritizing anti-racist and decolonized practices which are as relevant as having safe medical instruments and effective medications. As health delivery programs work towards decolonized practices, childbearing people can reclaim rights to their bodies and cultivate healthier relationships to their bodies. Trusting connections between clients and providers that prioritize individual autonomy are paramount for healing. “Growing Indigenous midwifery and supporting the training of Indigenous midwives is an ultimate goal for many stakeholders on-island. An out-of-hospital birthing space has been identified as a priority for community members in the North as well.” Dr. Gordon Horner, general practitioner, Daajing Giids “When I arrived in the year 2000, we (medical staff) were all supportive of on island delivery but for a certain period, there were no nurses with enough obstetrics training so birthers were told to go off island. Before the mid-1990s, it was a given that nursing staff would have been trained in birthing but then nurse education changed and it was optional to add obstetrics training. When studying to become a general practitioner, you only see obstetrics a few months in undergraduate and about three months of work as a resident. That wasn’t enough to be able to offer safe childbirth in our remote, isolated setting. “Childbirth care on Haida Gwaii was revolutionized when it shifted to a midwifery-led, hospital-supported system which maintains a very safe and supported birther-centered care system. Our system was improved through mentoring and training of nursing staff – midwives have been teaching staff birthing skills, showing them how to deal with their emotions and normalize births so they feel more comfortable with birthing. Most nursing staff have not had exposure to this type of birthing situation on island which is very different as there are no surgeons and little staff or several hours to reach a specialist. The fact is that since midwives have taken the first seat, I haven’t had to catch a baby and have only acted as an available back up for home deliveries. I’m very happy with where we’ve gotten, we have a real sense of shared vision and are all on the same team.”
“We’ve come a long way since the days of twilight sleep (which rendered the birthers unconscious or semiconscious) and forced supine position labouring, but there are still unfortunately accounts of birthers being pressured during their most vulnerable state to follow hospital protocols or undergo procedures that they feel they don’t have adequate knowledge about. The staffing shortages that the medical system is currently facing can also add pressure on staff and birthers.” The only issue here is that birth is rarely timely and smooth. The mind-body-emotional connection of the birther is the mechanism that births the baby. Our stress hormones block our birthing hormones, so if the birther cannot find an environment where they feel safe and relaxed, the birth is potentially at risk for intervention. “The message I would like to convey is that the birther plays the most central role in birth, and the nature of female cycles and birth are at odds with our capitalist system. I don’t know what it takes to change this, but I believe we can do it. The benefit of positive birth experiences (which can still happen with interventions) is immeasurable and far reaching and that is why I do this work.”
|




 Carsen Gray LaPlante, Birther of three children, Hl
Carsen Gray LaPlante, Birther of three children, Hl Jessiquita Madrid, Birther of one child, Daajing Giids
Jessiquita Madrid, Birther of one child, Daajing Giids  Anne-Marie Cayer, Midwife in Daajing Giids
Anne-Marie Cayer, Midwife in Daajing Giids 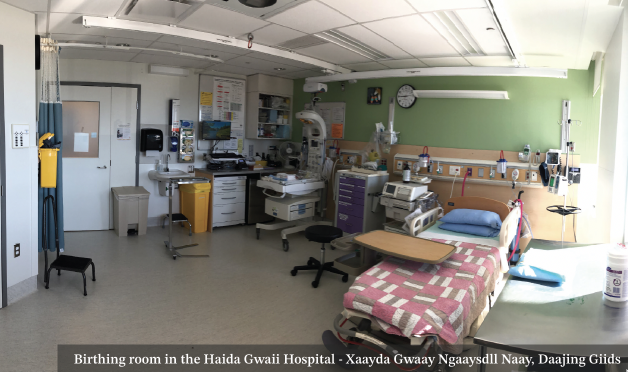
 Emily Campbell, doula, Masset
Emily Campbell, doula, Masset